Hypertension is defined as a chronic increase in systemic arterial pressure, with maximum (systolic), minimum (diastolic) or both values. Hypertension is often associated with metabolic disorders and functional and/or structural changes in target organs (such as the heart, brain and kidneys), and is aggravated by the presence of other risk factors such as dyslipidemia (changes in cholesterol and triglycerides), abdominal obesity, glucose intolerance, and diabetes mellitus (DM).
Arterial hypertension (HA), which has been classified by the World Health Organization (WHO) and incorporated into the Brazilian Hypertension Guidelines (2016), distinguishes the following categories:
Classification of Arterial Hypertension (> 18 years of age)
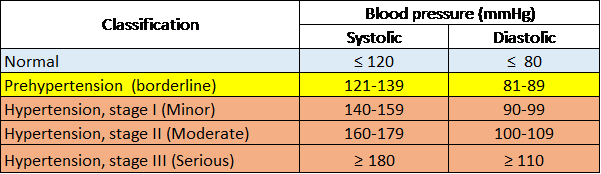
Sociedade Brasileira de Hipertensão [Brazilian Society of Hypertension], 2016.
Essential arterial hypertension (without a precise cause) accounts for at least 90% to 95% of all forms of hypertension. All other forms of hypertension, called secondary hypertension, are associated with some other disease and comprised between the remaining 5% and 10%. In this second group, hypertension of renal origin and the various forms of endocrine hypertension (hyperaldosteronism, Cushing's disease, and pheochromocytoma) prevail.
Systemic arterial hypertension affects about 20% of the population in Western countries and causes serious problems over time.
In Brazil, hypertension affects 32.5% (36 million) adults, more than 60% of whom are elderly, contributing directly or indirectly to 50% of cardiovascular deaths. Along with diabetes, its complications (heart, kidney and brain) significantly impact work productivity and family income, estimated at US$ 4.18 billion between 2006 and 2015.
Arterial hypertension has a family component. About half of all hypertensive patients have a family history of hypertension or premature cardiovascular mortality in their first-degree relatives.
Environmental Factors
The relationship between sodium content in the diet and blood pressure levels has been widely demonstrated. Arterial hypertension seems to be unknown among populations that consume little salt.
Although many doctors are convinced that stress can contribute to blood pressure, this remains a controversial issue.
Age & Gender
In industrialized countries, the average blood pressure of the population increases with age. After the age of 50, diastolic blood pressure tends to normalize and sometimes to decline,
while systolic blood pressure continues to rise to a later age.
Women are at an increased risk of developing hypertension after menopause.
Obesity
A correlation has been demonstrated between increased blood pressure values and increased weight and, conversely, a reduction in blood pressure as weight decreases in the obese.
Clinical Aspects of Hypertension
Physical condition is typically poor with no specific symptoms or signs of isolated hypertension, especially mild hypertension.
Headache (cephalea), vertigo and ringing in the ears are often considered as early and frequent symptoms of hypertension, although not specific. Oppressive and non-pulsatile headache, especially in the morning or at night, is reported by about 50% of hypertensive patients and is reduced by about half when the condition is treated. Niccturia (nocturnal urination) and vertigo are also frequently reported in hypertensive patients (about one-third of cases).
Clinical research into signs of disease in other organs is fundamental, especially for the purpose of evaluating the course of hypertension. They form the basis for the risk assessment of hypertension sufferers, since these signs indicate if arterial hypertension has begun to harm the brain, heart (muscle and coronary arteries) and kidneys.